When it comes to your health, seeing blood in the toilet after passing a bowel movement can be very concerning. In some cases, this could be a symptom of internal hemorrhoids, also known as piles. But in other cases, rectal bleeding could be a sign of cancer. As such, determining the cause of blood in the toilet could be critical to your long-term health. This post will help you determine whether your rectal bleeding is caused by hemorrhoids or cancer.

Blood in Toilet: Color Matters
When you notice blood in the toilet when wiping or after passing a bowel movement, taking careful note of the coloring could help determine the cause of this symptom. As this viral TikTok video recently helped clarify, the color of the blood could help you determine the cause of the bleeding.
If your rectal bleeding is the result of hemorrhoids symptoms, the blood will be bright red in color, much like pizza sauce fresh out of the jar. In contrast, blood related to colorectal cancer may be darker in color.
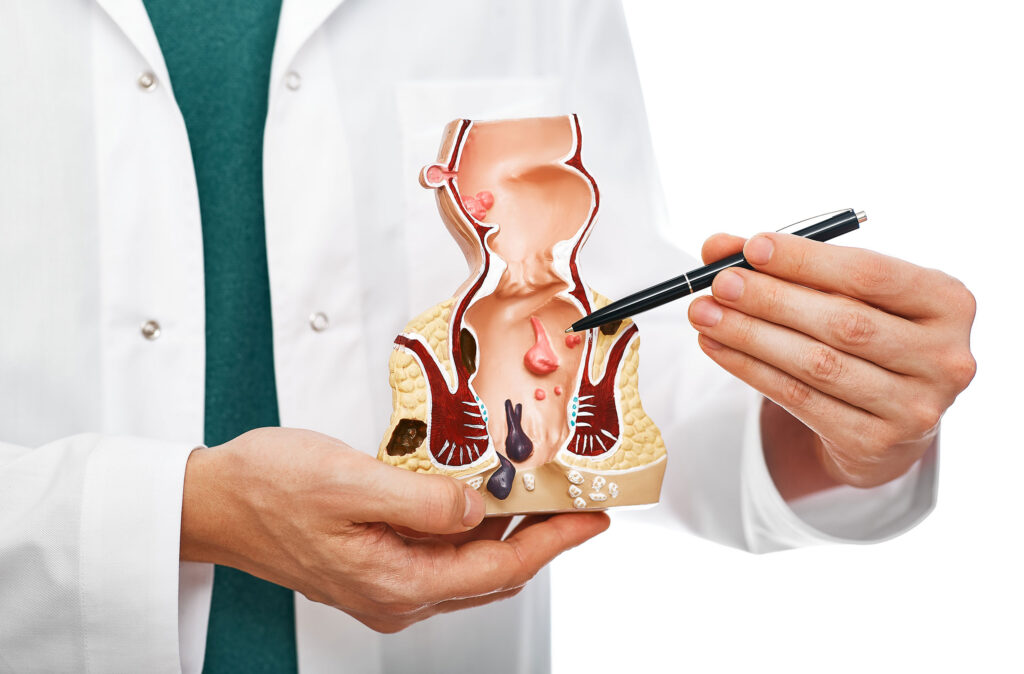
In addition to rectal bleeding, both hemorrhoids and anal or colorectal cancer can cause protrusions in the anus, as well as changes to your bowel habits. While closely monitoring the color of the blood you see in the toilet, the best way to get an accurate diagnosis is to see a trusted healthcare provider. After, you can begin seeking appropriate treatment.
Hemorrhoid Relief in Houston and Dallas
If internal hemorrhoids are determined to be the cause of blood in the toilet, topical products may help temporarily. However, once you have bleeding, your hemorrhoids are likely severe enough that only a medical procedure will provide lasting relief. In such cases, we encourage you to visit us at the Texas Hemorrhoid Institute by requesting a consultation [/tx-appt-link.] In one of our Houston or Dallas area offices, we can review minimally-invasive treatment options such as HAE (hemorrhoid artery embolization) to help you find symptom relief without undergoing invasive surgery.
Because they can cause frightening symptoms such as bleeding from the anus, many people wonder, “Are hemorrhoids dangerous?” These inflamed blood vessels that form in or around the rectum and anus typically do not pose a serious health risk. Rather, most hemorrhoid symptoms are merely intrusive and interfere with your quality of life.
But what happens if you don’t treat them? This post explains what happens if you leave them untreated, highlights the potential dangers of bleeding hemorrhoids, and provides information on treatment for severe cases.
Can Hemorrhoids Kill You?
While hemorrhoids can be very uncomfortable and cause serious complications, they cannot kill you. Untreated, they may start bleeding, and, if irritation persists, the swollen blood vessels could burst, but that would still not create a life-threatening situation.
Some hemorrhoids may develop an internal blood clot (a condition referred to as thrombosed hemorrhoids.) In such cases, you could experience pain simply from sitting, stretching, or walking.
Finally, internal hemorrhoids may protrude from the anus (referred to as prolapsing). If the anal muscles tighten around the prolapsed hemorrhoid, its blood flow could be restricted, resulting in strangulation and more discomfort. While all these complications can be very painful and worrisome, they are still not deadly.
The Dangers of Bleeding Hemorrhoids
If you’ve experienced rectal bleeding, or noticed blood in your stool due to hemorrhoids, you may wonder, “can you bleed out from hemorrhoids?” While you cannot, if bleeding is heavy and left untreated, you could develop anemia, a condition in which you don’t have enough red blood cells to distribute oxygen throughout your body.
What Happens if You Don't Treat Hemorrhoids?
Are hemorrhoids dangerous if left untreated? These swollen vessels in or around the rectum and anus rarely pose a serious health threat. But if left untreated, they may cause complications such as thrombosed, prolapsed, or strangulated hemorrhoids. Untreated, they may also bleed enough to make you anemic.
Additionally, hemorrhoids can impact your daily life, making it difficult for you to comfortably sit, concentrate at work, or engage in your favorite physical activities. In this scenario, it may be more difficult to maintain personal hygiene and keep yourself clean after passing a bowel movement.
Having this condition may also impact your bowel habits, contributing to constipation or even causing bowel incontinence.
Finally, your mental health may be impacted by your condition, as you experience the disruptions of symptoms such as pain, itching and bleeding from the rectum.
When Should You See a Doctor for Hemorrhoids?
Mild cases may resolve on their own within a few days, especially with lifestyle modifications. For example, increasing your fluid and fiber intake can soften your stool and reduce pressure on your lower rectum.
You can also try to engage in more physical activity, since remaining sedentary is a known risk factor for hemorrhoids.
However, you should see a doctor if:
- Your symptoms don’t resolve within a week.
- Your symptoms worsen.
- You notice blood in your stool.
- You are experiencing bleeding before, with, or after passing a bowel movement.
Symptomatic grade 2-3 internal hemorrhoids can respond to non-surgical hemorrhoids treatment options such as Hemorrhoid Artery Embolization. This minimally invasive procedure, available at the Texas Hemorrhoid Institute, shrinks them and reduces your symptom burden by cutting off blood supply to the swollen arteries.
So, are hemorrhoids dangerous? While they won’t kill you, they can take a toll on your quality of life and could cause serious complications. Seeking treatment can help provide relief, so request a consultationrequest a consultationrequest a consultation with our specialists today.
You can develop hemorrhoids from lifting weights if you lift too heavy or use incorrect form. If you already have them and are lifting weights, you might make your condition worse.
In this blog post, we cover how lifting weights leads to hemorrhoids, how to prevent them, and treatment options.

Can You Get Hemorrhoids From Lifting Weights?
If you lift weights using the wrong technique, you may develop new ones or worsen existing piles. (Remember, hemorrhoids are blood vessels in or around the anus and rectum that develop swelling after coming under excess pressure.) Weightlifting and this condition don’t have to go hand in hand, but lifting weights can cause hemorrhoids in several different ways.
Going too heavy
Can you get hemorrhoids from lifting? When weights are too heavy, you may strain to pick them up, putting pressure on your abdomen, lower rectum, and the blood vessels in those areas. Under that pressure, the veins can swell, causing hemorrhoids to form, or worsening existing symptoms if you already have piles.
Using the wrong form
You can get them from working out with weights if you aren’t careful about your form.
Cycling, squatting, and sit-ups
In addition to lifting weights, other forms of exercise may increase your risk. Use caution when cycling, since the hard seat of a stationary or outdoor bike can irritate existing ones.
Squatting can also increase your risk, especially if you hold weights while exercising, since the combination piles pressure on your lower body, including your rectum.
Sit-ups and crunches may even lead to the formation of hemorrhoids due to their potential to irritate the veins in and around the rectum.
How to Prevent Hemorrhoids When Lifting Weights
While you can get them from lifting weights, these tips can help protect you while you exercise.
Before starting to lift, bend your knees and turn on your core while keeping your spine in a neutral position. Move up and down slowly and steadily, avoiding any jerky or abrupt motions. When you lift weights or engage in any form of exercise, breathe slowly and steadily, trying to exhale at the most challenging moment of the movement.
If you’re just getting into weightlifting, or you haven’t worked out in a while, ease yourself into your routine, starting with lower weights and sticking to between 8 and 12 reps in each lifting set.
Also, make sure to engage in cross-training, trying different workouts all week to build up the muscles that support your weightlifting and to take some pressure off your rectum.
Focus on hydration, especially after a training session, to replenish fluids lost during your workout. Doing so will help prevent constipation and soften your stool, reducing your risk for developing hemorrhoids from weightlifting.
You can snack on fiber rich foods after a lifting session, focusing on choices such as nuts, since their combination of fiber and protein can reduce risk while supporting muscle growth and post-lifting recovery.
Seeing a Doctor for Your Hemorrhoids
While not typically dangerous, they can make you feel itchy or uncomfortable; they can also lead to bleeding when you pass bowel movements. As such, you should see a doctor when your symptoms are noticeable, as hemorrhoids treatment can provide relief and improve your quality of life—not to mention your weight-lifting routines.
Here at the Texas Hemorrhoid Institute, our interventional radiologists provide minimally invasive treatment options. Conduction the Hemorrhoid Artery Embolization (HAE) procedure, they can shrink cases without surgery and with a reduced risk for complications. Schedule a consultationSchedule a consultationSchedule a consultation today to explore this treatment option.
Hemorrhoids are swollen blood vessels that form in and around your rectum or anus due to pressure. While they are common and typically harmless, the symptoms sometimes overlap with those of colorectal cancer and anal cancer.
This post will help clarify the differences and answer the question, “Can hemorrhoids cause cancer?”

Can Hemorrhoids Be Cancerous?
No, hemorrhoids are not cancerous.
External ones cause symptoms such as lumps near the anus, pain, itching and swelling. Internal cases are typically less painful but may cause symptoms that mimic those of certain cancers, such as bleeding from the rectum or having bright red blood in the stool; mucus leaking from the anus; anal itching; and hemorrhoid protrusion from the rectum.
As a result, some people wonder if they can be cancerous, and the answer is no.
Still, it’s important to see your healthcare provider to find out.
Are Hemorrhoids a Sign of Cancer?
As mentioned above, hemorrhoids are not cancerous and they are not a sign of cancer. But symptoms can overlap with those of colon cancer and anal cancer.
Symptoms of colon cancer
Each year, approximately 150,000 Americans are diagnosed with colorectal cancer, a disease that can affect the colon or the rectum. While the disease is more common in people over the age of 45, it can develop in men and women of any age.
Common symptoms include:
- Rectal bleeding, a symptom shared with internal hemorrhoids
- Ongoing discomfort in the abdomen
- New weight loss, without a clear cause
- Changes in bowel movements
- Fatigue
- Weakness
Symptoms of anal cancer
Anal cancer is less common than colon or rectal cancer; it develops in your anal canal or anus and is almost always connected to a prior infection of Human Papilloma Virus (HPV.) Anal cancer symptoms include:
- Bleeding from the anus
- Abnormal anal discharge
- Itching surrounding the anus
- Having a mass or lump form at the anal opening
- Feelings of pain or fullness in the anal region
- Bowel movement changes
- Loss bowel control
- Anal or groin lymph node swelling
Can Hemorrhoids Turn Into Cancer?
Bleeding from the anus and discomfort are common symptoms of hemorrhoids, colon cancer and anal cancer. But these symptoms will look different with each condition.
- With hemorrhoids, the blood is typically bright red and mostly presents during or after a bowel movement.
- Bleeding associated with colorectal cancer can happen at any time, and the color of blood may me bright or dark red.
- Anal cancer-linked bleeding may also occur at any time. The blood could be black or bright red, and could have a tar-like consistency.
Using this guide could help distinguish between a piles and cancer diagnosis. But can untreated hemorrhoids lead to cancer? Or can they cause cancer? While they do not turn into or directly cause cancer, this study reveals that having piles increases your risk for developing colorectal cancer in the future. As such, seeking timely hemorrhoids treatment can bring symptom relief in the short term, while reducing your long-term risk of developing cancer.
When to See a Doctor About Your Hemorrhoids?
While hemorrhoids are unlikely to be cancerous, leaving them untreated can lead to reduce your quality of life while increasing your risk for infection and future cancer development. Plus, since some people struggle to differentiate between symptoms of hemorrhoids or colon cancer, promptly seeking the advice of a healthcare provider is the best way to protect your long-term health.
Today, it is possible to treat them without surgery, thanks to minimally invasive Hemorrhoid Artery Embolization (HAE), available at the Texas Hemorrhoid Institute. Request a consultationRequest a consultationRequest a consultation today to see if you’re a candidate for HAE.
When an internal or external hemorrhoid is too filled with blood, it may burst, causing discomfort and bleeding. This post explains what causes them to pop, how to treat a burst hemorrhoid, and when to seek medical attention.

What Happens When Hemorrhoids Pop?
When hemorrhoids become thrombosed, meaning a blood clot forms with the swollen vessels located in or around the rectum and anal opening, they may burst. (Both external and internal hemorrhoids can pop.) If that happens, you may notice bright red blood in your stool, on your toilet paper when you wipe, or in the bowl of the toilet.
In some cases, a ruptured internal hemorrhoid or popped external hemorrhoid can lead to heavy or continuous bleeding; the passing of large blood clots; and severe pain. In such cases, you should seek medical attention in order to prevent complications.
Is a Ruptured Hemorrhoid Dangerous?
While hemorrhoids can pop, the bursting does not usually pose a serious threat to your health. Rarely, a burst hemorrhoid can lead to ongoing bleeding from the rectum, which could cause adverse health complications if left untreated. Additionally, while bleeding from the rectum is a possible side effect of burst cases, this symptom could also be a sign of colorectal or anal cancer. As such, you should always discuss rectal bleeding with your healthcare provider.
Can Hemorrhoids Burst During Labor
Pregnancy is a risk factor for developing hemorrhoids, as the weight of your growing fetus and the increased blood volume in your body puts added pressure on your lower rectum. As such, many women worry and wonder, can they burst during labor?
During labor, straining and pushing to deliver your child can cause them to form, or worsen existing swelling in the vessels in and around your rectum. This can lead to thrombosed hemorrhoids—especially if you push for longer than 20 minutes—as all that strain directs additional blood into the veins surround the anus. And, since this type are subject to bursting, this increases the chances that a hemorrhoid will pop during labor.
How to Treat a Burst Hemorrhoid
If a hemorrhoid bursts, you may experience bleeding that lasts anywhere between a few seconds to a few minutes. Bleeding after passing a bowel movement may also persist for a few days. Most burst hemorrhoids won’t require medical treatment, although you can reduce any discomfort by soaking the area in three to four inches of warm—not hot—water, for between 15 and 20 minutes. In addition to soothing pain and inflammation, this soak can direct additional blood flow to your rectal area, helping speed the healing process for your burst hemorrhoid.
But what if your burst hemorrhoid bleeds for longer than 10 minutes? In such cases, you should be evaluated by a health care provider to make sure that you’re dealing with a burst hemorrhoid and not a different medical condition. Mention additional symptoms such as changes in the color or consistency of your stool; changes in your bowel movement habits; stomach pain or pain in the anal area; nausea, vomiting or weight loss; lightheadedness or dizziness; and/or fever. All of these symptoms could indicate other conditions that will require further medical interventions.
Final Thoughts
Can they burst? Yes. But seeking timely hemorrhoids treatment should prevent this outcome. And, if you wish to address grade 2 – 3 internal hemorrhoids without surgery, the experts at the Texas Hemorrhoid Institute are here to discuss Hemorrhoid Artery Embolization (HAE), a minimally invasive procedure that shrinks them by blocking their blood supply. Request a consultationRequest a consultationRequest a consultation today to explore your HAE candidacy.
If you struggle with hemorrhoids for over a year, you might have chronic hemorrhoids. Typically, these swollen vessels in or around the rectum resolve quickly. However, if you have chronic internal hemorrhoids or long-term symptoms, medical intervention may be necessary. This post provides an understanding of chronic hemorrhoids, including causes, symptoms, and treatment options.

What Are Chronic Hemorrhoids?
Small hemorrhoids will often resolve within a few days. However, persistent symptoms can last for over a year or more, becoming a chronic concern and impacting quality of life until you seek hemorrhoid treatment.
Symptoms of Chronic Hemorrhoids
Chronic hemorrhoids, the result of ongoing swelling in the blood vessels of your rectum or anus, most commonly lead to persistent symptoms such as itching, discomfort and bleeding. Other symptoms may include
- Irritation and pain in the area surrounding the anus
- The formation of a hard lump or swelling around your anus
- Bleeding or pain with bowel movements
- Noticing bright red blood in your stool, in the toilet bowl or on your toilet paper
- Aching pain in the anus, particularly when sitting down
- Prolapsing from the anus (when an internal hemorrhoid pops out of your anal opening. In some cases, a prolapsed hemorrhoid can be repositioned manually. But if you have grade 4 hemorrhoids, indicating the most severe symptom burden, prolapsing may not be resolved without medical intervention.)
Chronic hemorrhoids can also become thrombosed—that means a blood clot has formed inside the swollen vessels. In turn, they may burst, resulting in temporary discomfort and bleeding or, in some cases, prolonged bleeding that requires medical attention.
Treatment Options for Chronic Hemorrhoids
While chronic hemorrhoids can last for over a year without intervention, even the most persistent should respond to treatment. And the treatment option you select will likely be based on the severity of your symptoms.
How to Get Rid of Chronic Hemorrhoids
Internal hemorrhoids are graded on a scale of 1-4, based on the severity of prolapse. If you have grade 1, you may be able to relieve symptoms and resolve swelling in the blood vessels by changing your lifestyle and using over-the-counter products, even if you have had them for over a year.
Start by drinking more fluids and eating more foods that are rich in fiber. This can help soften your stool, making it easier to pass bowel movements and helping reduce pressure on your lower rectum.
At the same time, while you’re dealing with persistent symptoms, you can relieve itching and discomfort with products such as hemorrhoid creams or soothing witch hazel wipes. Try to limit the amount of time you spend sitting on the toilet, and cleanse yourself gently after passing a bowel movement to reduce irritation in the area.
Once hemorrhoids have been classified as grade 2 or 3, lifestyle measures alone may not provide sufficient symptom relief. In such cases, a medical procedure such as Hemorrhoid Artery Embolization (HAE) can shrink them by cutting off their blood supply. Performed as an outpatient procedure, without large incisions, general anesthesia or overnight hospital stays, this minimally invasive procedure can provide lasting hemorrhoid relief with less downtime and a reduced risk for complications.
Once you have grade 4 hemorrhoids, you are unlikely to be a candidate for HAE. Instead, you may need to surgically remove them order to resolve symptoms and find lasting relief.
When to See a Doctor for Chronic Hemorrhoids
When hemorrhoid symptoms last longer than a few weeks, or when you experience any type of bleeding from the anus, it’s time to see your healthcare provider and discuss treatment options.
Allowing hemorrhoids to persist without intervention could allow symptoms to progress, leaving you with fewer treatment options. We invite you to request a consultationrequest a consultationrequest a consultation at the Texas Hemorrhoid Institute to explore your candidacy for minimally invasive HAE.
Having hemorrhoids can cause changes in the way you pass bowel movements, and they may contribute to constipation. If symptoms are mild, hemorrhoids will not affect your bathroom habits. However, when symptoms are more disruptive, they can cause bowel issues.
In this article, we explain the relationship between constipation and hemorrhoids, including prevention tips and treatment options.

The Role of Constipation in Developing Hemorrhoids
Do hemorrhoids make you constipated? Yes, they can contribute to constipation. However, the reverse is also true: chronic constipation increases your risk for developing them (also known as piles.)
With constipation, you will likely need to strain in order to pass a bowel movement. The force of that straining increases pressure on the lower rectum and anus, and that pressure can cause veins in the area to swell, leading to hemorrhoid formation. (If the veins inside the rectum become swollen, you will develop internal cases. When vessels outside the rectum or anus are affected, they form externally.)
Once they’ve formed, they can trigger symptoms such as pain, itching and rectal bleeding. In turn, you may delay or avoid trying to pass stool, even when you feel the urge to go. Unfortunately, holding in a bowel movement can cause the stool to harden, becoming more difficult to pass and contributing to constipation. Furthermore, if they are severely swollen, the piles could partially block your anal opening, making it harder to pass stool and causing you to strain harder when using the toilet, causing constipation or worsening existing bowel issues.
How to Treat Constipation and Hemorrhoids
While hemorrhoids can cause constipation, you may be able to alleviate both concerns by engaging in lifestyle-based hemorrhoids treatment such as changes in diet and exercise levels. Start by increasing the amount of water you consume, since this can help soften stool, reducing the need to strain in the bathroom and making it easier to pass a bowel movement.
Adding additional soluble fiber to your diet will also soften stools—great food-based fiber sources include black beans, Brussels sprouts, avocados and pears. If you struggle to meet your ideal daily fiber intake through diet (women should aim for 25 grams each day, while men’s recommended daily intake is 38 grams), supplements can also be helpful.
Exercise may also help alleviate both constipation and the condition. (Leading a sedentary lifestyle is considered a risk factor for hemorrhoid development.) Even something as simple as a daily walk can help support better bowel health and may relieve mild hemorrhoid symptoms.
Other Ways Hemorrhoids Can Affect Your Bowel
In addition to contributing to constipation, can hemorrhoids cause bowel issues of other kinds? When piles are large and swollen, several different bowel issues can become a problem.
Bowel incontinence
Large, swollen piles can prevent complete closure in the muscles surrounding your anus. As a result, they can cause bowel incontinence in the form of leaking stools or mucus coming from the anal opening.
Affected bowel movements
Hemorrhoids can affect bowel movements in multiple ways. As reviewed, both external and internal cases can contribute to constipation. Larger, swollen piles can interfere with anal function, allowing for involuntary stool leakage. Having internal ones can make you feel like there is stool stuck in your anus and can cause bleeding when you pass a bowel movement, or lead to bright red blood appearing in your stool.
Piles can create an uncomfortable feeling of fullness, making it feel like you have to use the bathroom, even when you’ve just passed a bowel movement. And having this condition can make it painful to pass any kind of bowel movement.
Having hemorrhoids can cause constipation, along with other changes to your bowel movements. Additional symptoms may include pain, itching and bleeding. When symptoms are mild, you may be able to find relief with lifestyle-based interventions, as well as over-the-counter hemorrhoid products.
However, when symptoms are more severe, or when you have grade 2-3 internal hemorrhoids, electing to have a medical procedure will be a more effective option. Request a consultationRequest a consultationRequest a consultation at the Texas Hemorrhoid Institute, and learn more about Hemorrhoid Artery Embolization, a less-invasive hemorrhoid treatment option.
Hemorrhoids are merely swollen, inflamed vessels that form in and around the anal opening. However, certain hemorrhoid symptoms are similar to the symptoms of anal cancer and other disease. As such, some people may conflate the side effects of hemorrhoids with cancer. But there are simple ways to detect the differences, and this post will help lead you to specialists who can give you a proper diagnosis.

Symptoms of Hemorrhoids
Hemorrhoids can form externally, meaning outside of the anus, causing itching, swelling and discomfort. And, when they form internally, they may not be painful but hemorrhoid symptoms there may include rectal bleeding, the leakage of mucus, itching or even protrusion.
Symptoms of Anal Cancer
Again, while hemorrhoids aren’t a sign of cancer, the two conditions share common symptoms. In fact, according to the American Cancer Society, symptoms of anal cancer include bleeding from the anus, abnormal discharge from the anus and itching around the rectum, all symptoms that are also associated with hemorrhoids. However, unlike hemorrhoids, anal cancer can also cause:
- A lump or mass to form at the opening of your anus
- A feeling of pain or fullness in your anal region
- Changes to your bowel movements
- Loss of control over your bowels
- Swelling of the lymph nodes in your anus or groin
Hemorrhoids & Cancer: When to See a Doctor
Mild hemorrhoid symptoms may be resolved with homecare and lifestyle changes, including increasing your fluid and fiber intake to reduce constipation, making it easier to pass bowel movements and reducing pressure on your anus and rectum. At the same time, you should avoid sitting on the toilet for too long, or straining to pass a bowel movement. And, even if your stools are loose, try to address diarrhea as frequently passing stool can also irritate your anal region and contribute to hemorrhoid development.
However, if your symptoms persist or worsen, or if you experience any rectal bleeding, you should see a doctor right away. When you see a healthcare professional, you can distinguish hemorrhoids and cancer symptoms. Then, if internal hemorrhoids are to blame for your discomfort, you can request a consultation request a consultation request a consultation with the Texas Hemorrhoid Institute to discuss your treatment options.
Swelling in the blood vessels and tissue in and around your anus causes hemorrhoids, also known as piles, to develop. These bulging vessels can cause symptoms such as discomfort, itching and even bleeding when you pass a bowel movement, depending on their severity. But do hemorrhoids cause gas or other abdominal symptoms? Here’s what you need to know.

Do hemorrhoids cause gas?
Having hemorrhoids will not directly cause gas and bloating. However, if you have internal hemorrhoids, they can impact your ability to comfortably pass stools or gas. As such, you may notice gas building up and causing discomfort, along with bloating.
Addressing gas caused by hemorrhoids
When gas buildup is caused by infrequent bowel movements, adding fiber to your diet could help relieve constipation and bloating. You should also avoid habits that are known to increase the buildup of gas, such as chewing gum or talking while you drink and eat. Finally, you may be able to relieve multiple hemorrhoid symptoms by focusing carefully on your diet.
Specifically, you can eliminate foods that can increase gas buildup, including:
- High fructose corn syrup
- Sweeteners such as sorbitol and erythritol
- Dairy products
- Legumes such as beans and chickpeas
- Whole grains
- Vegetables such as broccoli, cabbage and cauliflower
Additional hemorrhoid symptoms
In addition to gas and bloating with hemorrhoids, you may experience symptoms such as pain, itching or noticing bright red blood in your stool. Additionally, internal hemorrhoids may protrude from your anus, known as prolapsing. Sometimes, you may be able to manually reposition the swollen vein, but in other cases, the prolapsed hemorrhoid can only be resolved with medical intervention.
When to Seek Hemorrhoid Treatment
While mild hemorrhoids may resolve on your own, it’s never too soon to try and address piles. After all, mild hemorrhoid symptoms can be relieved with home care, but as the symptom severity increases, the solutions become more invasive.
To begin with, you may be able to find relief by following this diet to help hemorrhoids and reducing the amount of time you spend sitting, especially on the toilet. Soaking in warm, shallow water can soothe inflamed hemorrhoids. And you may benefit from an over-the-counter hemorrhoid cream if your symptoms are still mild.
When you pass stool, try to gently pat the area clean and avoid vigorous wiping, or use soothing medicated wipes instead of rough toilet paper. If you are carrying extra weight, reducing your BMI may help, since there’s a connection between obesity and hemorrhoids. And if you suffer from IBS and hemorrhoids, reducing flares can also help relieve your piles symptoms.
However, if you have grade 2 or 3 internal hemorrhoids, you may need a medical procedure to find symptom relief. In such cases, you can avoid surgery by choosing to undergo hemorrhoid artery embolization (HAE), a minimally invasive procedure that shrinks hemorrhoids by cutting off their blood supply. And you can request a consultation request a consultation request a consultation at the Texas Hemorrhoid Institute to see if you’re a candidate for HAE.
Many people with IBS (irritable bowel syndrome) develop hemorrhoids, often because they’re sitting on the toilet too long due to constipation or diarrhea. But do IBS and hemorrhoids always go hand in hand? And can you manage your symptoms to reduce your risk for hemorrhoids? Here’s what you need to know.

What is Irritable Bowel Syndrome?
IBS is a gastrointestinal disorder that can cause constipation (IBS-C), diarrhea (IBS-D) or a mixture of symptoms (IBS-M). The exact causes of IBS are not well-known. But, in addition to changes in your bowel movements, symptoms can include:
- Bloating
- Gas
- White mucus in the stool
- Feeling like your bowels aren’t emptied, even after passing stool
What’s the Connection Between IBS and Hemorrhoids?
Research suggests that IBS increases your hemorrhoid risk, largely because many IBS symptoms are part of what causes hemorrhoids. Plus, if you already have this problem, your IBS symptoms can make hemorrhoids symptoms worse.
But why is that true? IBS sufferers with constipation often strain to pass bowel movements, causing rectal and anal veins to bulge and swell under the pressure. Even if you have diarrhea, and stools pass quickly, you’re still likely spending more time sitting on the toilet, increasing your risk for both internal and external hemorrhoids. And, if that happens, you may develop complications including:
- Bleeding, especially when you pass stool
- Itching
- Prolapsed hemorrhoids
- Strangulated hemorrhoids
- Urinary retention (difficulties completely emptying your bladder)
Fortunately, you may be able to manage IBS and hemorrhoids with simple lifestyle changes, including changes to your diet.
Managing IBS and Hemorrhoids with Diet
When you have IBS, you should steer clear of trigger foods such as beans, dairy products, spicy foods, alcohol and sorbitol, mannitol, or xylitol. If you struggle with constipation, you may find relief by taking in more fluid and fiber. But be aware that certain fruits and vegetables may trigger worsening IBS symptoms. And, since lifestyle changes won’t relieve all cases of IBS and hemorrhoids, you may need to seek further hemorrhoid treatment.
Finding Hemorrhoids Relief in Texas
If your IBS diagnosis has left you facing the symptoms of grade 2 or 3 internal hemorrhoids, help is available at the Texas Hemorrhoid Institute. Our interventional radiologists provide a medical procedure—called Hemorrhoid Artery Embolization, or HAE—that provides a less invasive alternative to hemorrhoid surgery while still resolving painful symptoms. Best of all, the procedure allows you to avoid overnight hospital stays, and it comes with a shorter recovery period and a reduced risk for complications. So, is HAE the right procedure to relieve your hemorrhoids? While not everyone is a candidate, we’re here to review your treatment options. So, to get the process started, we encourage you to request a consultation request a consultation request a consultation with our hemorrhoid specialists in Houston and Dallas.