If you've been living with internal hemorrhoids, you may already be dealing with painful, disruptive symptoms. And that may be impacting several areas of your life. But if you're wondering, can you have intercourse with hemorrhoids, here's what you need to know.

What are hemorrhoids?
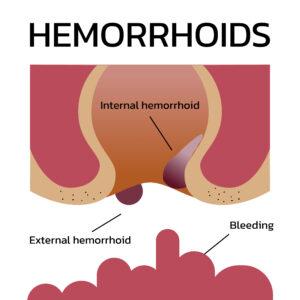
Hemorrhoids (or piles) are just enlarged veins in your rectum or anus. Sometimes, the walls of these vessels stretch very thin, causing bulging and irritation in the veins. Now, we classify your hemorrhoids according to the severity of your symptoms. You'll be diagnosed with:
- Grade 1 hemorrhoids
if they are small, and not visible or palpable. While unlikely to cause discomfort, they may cause bleeding when you pass a bowel movement. - Grade 2 hemorrhoids
are larger, and may pop out of the anus when you pass a bowel movement. Symptoms can include pain, itching and bleeding. - Grade 3 hemorrhoids
are internal vessels that bulge outside your anal canal, and will not return unless you reposition them manually. They are also symptomatic. - Grade 4 hemorrhoids
are the most severe. The bulging vessels will stay outside the anal canal, even if you manually reposition them, and your symptoms are likely to be severe.
Can you have intercourse with hemorrhoids?
With more severe hemorrhoids, intercourse (either vaginal or anal) may be painful. Now, while this may prevent you from connecting with penetration, that doesn't mean you'll have to avoid intimacy altogether. Instead, you and your partner may need to find other ways to express your intimate connection. Then, once you relieve your discomfort with hemorrhoid treatment, you can return to your former sexual connections, following your recovery period.
Hemorrhoid Treatment in Texas
Here at the Texas Hemorrhoid Institute, we treat grade two and three internal hemorrhoids with Hemorrhoid artery embolization (HAE), a non-surgical procedure that relieves your symptoms with a fast recovery, reduced risk for side effects and minimal discomfort.
Wondering if you can have intercourse with hemorrhoids despite your pain, itching and bleeding? You may be able to connect with penetration without treatment. But you're more likely to enjoy intercourse, and the rest of your daily activities, by seeking relief via treatment. Ready to begin your recovery journey? Click here to request an appointmentClick here to request an appointmentClick here to request an appointment with our hemorrhoid experts in Texas.
Today, you can eliminate internal hemorrhoids without surgery by choosing Hemorrhoidal Artery Embolization (HAE). But what are hemorrhoids, and why would you choose this minimally invasive treatment option to relieve their symptoms? Here's what you need to know.

Understanding Hemorrhoids
Symptomatic hemorrhoids are also called piles. Basically, they are bulges in your rectum that form in spots of abnormal connections between arteries and veins. Before HAE was an option, patients needed to eliminate internal hemorrhoids via surgery. Today, however, embolization can relieve symptoms such as itching and bleeding by blocking blood flow to the affected arteries.
HAE to Eliminate Internal Hemorrhoids: What are the Advantages?
HAE is a popular alternative to surgery when it comes to treating internal hemorrhoids. In addition to being a lower cost treatment option, it also offers improved:
- Comfort, since we deliver treatment via a tiny puncture instead of a surgical incision
- Convenience, since you avoid overnight hospital stays and can walk out of your procedure
- Symptoms, since HAE offers results that compare to surgery, but without side effects and a lower risk for complications
Who is a Candidate?
You can consider HAE to eliminate internal hemorrhoids if your:
- Internal hemorrhoids have been classified as grade two or three
- Symptoms include heavy bleeding
- Internal hemorrhoid has prolapsed
Meet Our Experts
At the Texas Hemorrhoid Institute, our physicians in Houston and Dallas are dedicated to delivering outstanding patient care along with noticeable and lasting results. Our main goal is to ensure that you understand your treatment options, and that we partner together to find your perfect pathway to relief.
Click here to request an appointmentClick here to request an appointmentClick here to request an appointment today.

Is hemorrhoid embolization the same as hemorrhoidectomy? Well, while both are treatment options for hemorrhoids, these are very different procedures when it comes to invasiveness and post-procedural recovery. What is similar, however, are the procedures' success rates when it comes to providing hemorrhoid relief! How is that possible? Let’s find out, together!
What are hemorrhoids?
Symptomatic hemorrhoids, or piles, are just enlarged veins that form in your rectum and/or anus. In some cases, their walls stretch so thinly that they bulge and develop irritation. If you have hemorrhoids, they may be internal (forming in the lower rectum, above the anus); external (forming around the anus); or thrombosed (internal or external hemorrhoids that develop a blood clot.)
When you are hoping to treat your hemorrhoids, your condition will be described in terms of a grading system that’s based on severity. And the severity of your condition will help determine your ideal treatment option.
- Grade 1
These hemorrhoids are small, and you can’t usually see or feel them. Still, they can cause bleeding during bowel movements. - Grade 2 hemorrhoids may protrude outside your anus when passing a bowel movement, but typically return without assistance. Symptoms include pain, itching, discomfort and bleeding.
- Grade 3 hemorrhoids bulge outside your anal canal and won’t go back inside unless they’re physically pushed back. They also cause pain, bleeding, and itching.
- Grade 4 symptomatic hemorrhoids are so prolapsed that they won’t stay inside the anal canal even when manually repositioned. Symptoms are severe.
What is hemorrhoid embolization?
Hemorrhoid embolization, also referred to as hemorrhoid artery embolization (HAE) is a non-surgical treatment for symptomatic hemorrhoids. It’s a minimally invasive procedure with a high success rate, minimal discomfort, faster recovery and a lower risk for complications.
Candidates for HAE have internal hemorrhoids that are at stage 2 or 3, causing significant discomfort for the patient. In order to resolve this discomfort, the HAE procedure involves inserting a small catheter into the arteries that deliver blood to your hemorrhoids. Next, our Texas hemorrhoid specialists inject embolic material to these catheters, blocking the arteries and cutting off blood flow to the hemorrhoids. Without that blood supply, the hemorrhoids begin to shrink, eventually disappearing.
What is hemorrhoidectomy?
A hemorrhoidectomy is the surgical removal of internal or external hemorrhoids. It is typically reserved for patients with severe symptoms, and grade 3 or 4 hemorrhoids, since this surgery is associated with complications such as pain, bleeding, retention of urine, urinary tract infections and fecal impaction or incontinence.
Is hemorrhoid embolization the same as hemorrhoidectomy: exploring success rates!
Hemorrhoidectomy comes with a 95% success rate when it comes to treating severe hemorrhoids. But the procedure is also known to cause complications, and comes with an intense recovery procedure.
In contrast, HAE is also a very effective treatment option for internal hemorrhoids. (As a newer treatment options, long-term data is less readily available, so the numbers aren’t as exact.) However, clinical studies consistently demonstrate that HAE has a high success rate at treating internal grade 2-3 hemorrhoids, effectively reducing bleeding, itching, and discomfort while significantly improving your overall quality of life.
Even better? Compared to hemorrhoidectomy, HAE has a lower risk of complications. Plus, it’s commonly performed on an outpatient basis, meaning you can avoid an overnight hospital stay. And, because it’s a minimally invasive discomfort, HAE also minimizes your discomfort and recovery period. Finally, HAE is a more affordable treatment option, since it allows you to avoid long hospital stays.
So, to return to our original question: is hemorrhoid embolization the same hemorrhoidectomy? Well, if you have grade 2 or 3 hemorrhoids, here’s your answer: the relief they provide is likely to be the same, but the cost, pain and risk for complications is much lower for HAE than for hemorrhoidectomy.
Ready to find out if you’re a candidate for HAE in Texas? Click here to request an appointmentClick here to request an appointmentClick here to request an appointment

If you relief from internal hemorrhoids, it’s important to understand why they develop, plus how they can be prevented or treated. Here's what you need to know.
Internal hemorrhoids
These are invisible, swollen vessels that lie inside your rectum. While you you can’t usually feel the vessels, you can feel their effects, including:
- Bleed when passing a bowel movement. You may notice bright red blood on your toilet paper, but are unlikely to feel pain related to the bleeding.
- Prolapsing. An internal hemorrhoid may push through your anal opening, causing pain and irritation.
Root causes
Internal hemorrhoids tend to form when you put too much pressure on the veins around your anus, resulting in stretching and swelling. That pressure could result from:
- Straining to pass bowel movements.
- Sitting for too long, especially on the toilet.
- Chronic diarrhea or constipation.
- Obesity.
- Pregnancy
- Anal intercourse.
- Eating a low-fiber diet.
- Frequent heavy lifting.
Preventing internal hemorrhoids
Instead of helping you get rid of internal hemorrhoids, we'd love to prevent them from forming. And we can help do that by making it easy for you to pass bowel movements. And, to improve digestion and elimination, that end, we recommend eating high-fiber foods such as whole-grains, fruits and vegetables. Try to drink between six and eight glasses of liquid each day (more if you exercise) and, if your diet alone isn’t enough to pass stool with ease, you may need to include a fiber supplement in your diet.
Now, when you do need to pass your bowels, try not to strain or push. Also, get regular exercise, since movement can help avoid other risk factors for internal hemorrhoids, while encouraging you to drink additional fluids.
Treating Internal Hemorrhoids with HAE in Texas
When diet and lifestyle measures fail to prevent internal hemorrhoids, and you’re not ready, willing or able to undergo surgical treatment, hemorrhoid artery embolization is a great way to get rid of your problem! Ideal for patients with grade 1 to 3 internal hemorrhoids, this minimally invasive treatment option is performed as an out-patient procedure without general anesthesia or an overnight hospital stay. Click here to request an appointmentClick here to request an appointmentClick here to request an appointment with the Texas Hemorrhoid Institute.

Our interventional radiologists in Texas offer Hemorrhoidal Artery Embolization (HAE) for internal hemorrhoid treatment. It's a safe, clinically proven procedure that effectively treats hemorrhoids in a minimally invasive way.
But how does this work? Well, hemorrhoids are simply enlarged vessels; they develop because of abnormal connections between arteries and veins in the rectum. As such, by blocking blood flow to those vessels using embolization, we can shrink hemorrhoids and resolve symptoms such as itching and bleeding.
Why Choose HAE for Internal Hemorrhoid Treatment?
Today, many patients seek hemorrhoidal artery embolization (HAE) over other options because it allows them to find internal hemorrhoid relief while avoiding surgery. Plus, HAE offers:
Comfort
We perform HAE via catheter inserted through a pin-size access point on your leg. As such, you won't need general anesthesia or an overnight hospital stay. And you'll be able to go home on the same day as your procedure!
High success rate
Patients who choose HAE over surgery find comparable symptom relief, but with fewer side effects, making this a...
Lower risk internal hemorrhoid treatment
Unlike procedures such as a hemorrhoidectomy, rubber band ligation or infrared coagulation, HAE does not result in any reported side effects.
When Should You Come to the Texas Hemorrhoid Institute?
Good HAE candidates have:
- Been diagnosed with internal hemorrhoids
- Disruptive symptoms such as heavy bleeding
- Prolapsed internal hemorrhoids
Meet our Interventional Radiologist, Specializing in Internal Hemorrhoid Treatment
At the Texas Hemorrhoid Institute, Dr. Luke Carlson (a dual board-certified vascular and interventional radiologist) specializes in hemorrhoid artery embolization. With years of experience in this field, he welcomes patients seeking effective internal hemorrhoid treatment.
Under Dr Carlson's expert care, the Texas Hemorrhoid Institute offers effective hemorrhoid treatment solutions. Our hemorrhoid artery embolization procedure yields exceptional patient outcomes across age groups and diverse patient populations. Click here to request an appointmentClick here to request an appointmentClick here to request an appointment so we can determine if HAE is right for you.
What is hemorrhoid embolization? It's one of the newest, and least invasive, ways to find relief for internal hemorrhoids. But what are internal hemorrhoids, who is affected by this condition, and why does HE offer effective relief? Here's what you need to know!
Why internal hemorrhoids form
Internal hemorrhoids are swollen blood vessels that develop inside the rectum. Typically, that happens due to the pressure of constipation or when you strain to pass bowel movements. Symptoms include bleeding when you pass stool, as well as itching and/or mild discomfort.
When you have internal hemorrhoids, they're classified based on symptom severity, using a scale of grades 1 to 4 (1 is least severe). While not every patient experiences discomfort, most realize they have internal hemorrhoids when they see blood spots on the toilet paper or in the bowl.
What are my options for treating hemorrhoids?
If you have Grade 1 (or mild) hemorrhoids, you can usually find relief with lifestyle changes such as increasing water and fiber intake. However, with grades 2 through 4 hemorrhoids, you'll likely need medical intervention to find relief. In the past, that almost always meant surgery. However, over the last 10 years ago, we've perfected a new treatment option: hemorrhoid embolization. Backed by research, this minimally invasive treatment option provides equal or superior relief to surgical hemorrhoid removal. And, thanks to a shorter, easier recovery period, you face lower risks for complications.
What is hemorrhoid embolization?
Internal hemorrhoids involve the Corpus Cavernosum Recti (CCR) network of arteries and veins. So, by reducing CCR blood flow via embolization, we're able to also reduce the pain, pressure, itching and bleeding of internal hemorrhoids.
What should you expect during embolization? First, our interventional radiologists insert a small catheter through your wrist or groin. Using this tiny access point, we then guide that catheter to blood vessels in the rectum with the help of X-ray imaging. Once in place, we can then implant small coils in those blood vessels, reducing the flow of blood and your symptoms of internal hemorrhoids. Just about 45 minutes later, you'll be ready to go, returning to work the next day and avoiding an overnight hospital stay.
Success rates of hemorrhoid embolization
Despite being a 10-year-old procedure, current efficacy results are promising. One 2016 study followed 40 patients experiencing grade 1 to 3 internal hemorrhoids; one month after embolization, none experienced post-procedural complications, and 94% achieved relief.
By 2018, a more recent study followed 25 patients with grade 2 and 3 internal hemorrhoid patients, one year after a hemorrhoid embolization. Again, none experienced post-procedural complications. And 78% were still symptom-free, enjoying lasting hemorrhoid relief.
Hemorrhoid Embolization in Texas
While hemorrhoid embolization is safe and effective, it's only recommended for patients with grade 2 or 3 internal hemorrhoids. Before coming to our Texas Hemorrhoid institute, try lifestyle changes to see if they can provide relief. Then, if you still experience the pain, itching and bleeding of internal hemorrhoids, come and schedule a consult schedule a consult schedule a consultwith our interventional radiologists!

Why would you choose hemorrhoid embolization over other treatments for internal hemorrhoids? And are there other treatment options you should consider? This post breaks down all the important details.
Understanding hemorrhoids
These are swollen veins in your anus or lower rectum, and they can take two forms: internal (developing inside your rectum) or external (developing on the outside). While external hemorrhoids typically cause more pain, internal hemorrhoids may lead to itchiness, discomfort and/or bleeding.
In fact, chronic bleeding is the most common complaint associated with internal hemorrhoids. And that's why we see many patients coming into our Texas Hemorrhoid Institute who have noticed blood in their stool.
Hemorrhoid Treatment Options in Texas
There are several minimally invasive treatment options for internal hemorrhoids. Some involve changes in lifestyle including modifying your diet; others involve medication or injections; while still others include procedures like a rubber band ligation. However, these treatments fail to offer relief to at least 10% of internal hemorrhoid patients.
In the past, that meant your only remaining option was to schedule hemorrhoidectomy surgery. However, that procedure came with a higher risk for complications. Luckily, there's newer, better option available: hemorrhoid embolization.
What is Hemorrhoid Embolization?
For approximately 10 years, hemorrhoid embolization has offered minimally-invasive treatment for stage 1 through stage 3 level internal hemorrhoids. Unlike other treatment options, hemorrhoid embolization doesn't lead to anal incontinence and won't lead to rectal wounds. Plus, you don't lose the tissue surrounding those hemorrhoids, and you don't need general anesthesia or an overnight stay in the hospital. And, within three days of the procedure, most patients can resume all normal activities.
While these are all clear benefits, you may wonder, how long does hemorrhoid embolization last? Here again, the news is promising. Because the success rate for hemorrhoid embolization is about 90%, whereas many other treatment options come with 49% recurrence rates.
Looking for lasting relief from the discomfort, itchiness and bleeding of internal hemorrhoids, but hoping to avoid invasive surgery, major lifestyle changes or even the high likelihood of recurrence after treatment? Contact the Texas Hemorrhoid InstitueContact the Texas Hemorrhoid InstitueContact the Texas Hemorrhoid Institue to connect with our interventional radiologists. We'll schedule you for a consultation and determine whether you're a good candidate for hemorrhoid embolization.